In this article, “How to Test for Malnutrition Using Different Procedures,” the various methods of testing for malnutrition will be explored. From simple physical examinations to advanced laboratory tests, these procedures play a crucial role in identifying and addressing malnutrition. By understanding the different techniques available, individuals can gain insight into their nutritional status and take appropriate action to improve their overall health and well-being.
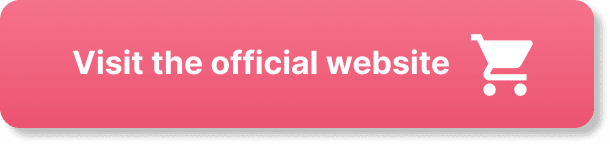
This image is property of malnutritionquality.org.
Understanding Malnutrition
Malnutrition is a condition characterized by a lack of proper nutrition, resulting in deficiencies or imbalances in essential nutrients needed for growth and overall health. It can occur when an individual does not consume enough nutrients or when the body is unable to absorb or utilize these nutrients effectively. Malnutrition can have severe consequences on physical and mental health, impacting growth, development, and immune function.
Definition of malnutrition
Malnutrition refers to a state of inadequate or excessive nutrient intake, which can lead to deficiencies or imbalances in essential nutrients necessary for overall health. This can include deficiencies in macronutrients like carbohydrates, proteins, and fats, as well as micronutrients such as vitamins and minerals.
Causes and consequences of malnutrition
There are various causes of malnutrition, including inadequate food intake, poor dietary choices, lack of access to nutritious foods, digestive disorders, and certain medical conditions. Additionally, factors such as poverty, food insecurity, and limited education about nutrition can contribute to malnutrition.
Malnutrition can have detrimental effects on both physical and mental health. It can weaken the immune system, leading to an increased susceptibility to infections and delayed wound healing. Malnourished individuals may experience stunted growth, muscle wasting, fatigue, weakened organ function, and impaired cognitive development. In severe cases, malnutrition can be life-threatening.
The linkage between malnutrition and diseases
Malnutrition can contribute to the development of various diseases and health conditions. For example, inadequate intake of certain nutrients like vitamin C can lead to scurvy, while insufficient protein intake can result in muscle wasting and weakened immune function. Long-term malnutrition can increase the risk of chronic diseases such as cardiovascular disease, diabetes, and compromised bone health. It is crucial to address malnutrition promptly to prevent these adverse health outcomes.
Common Signs and Symptoms of Malnutrition
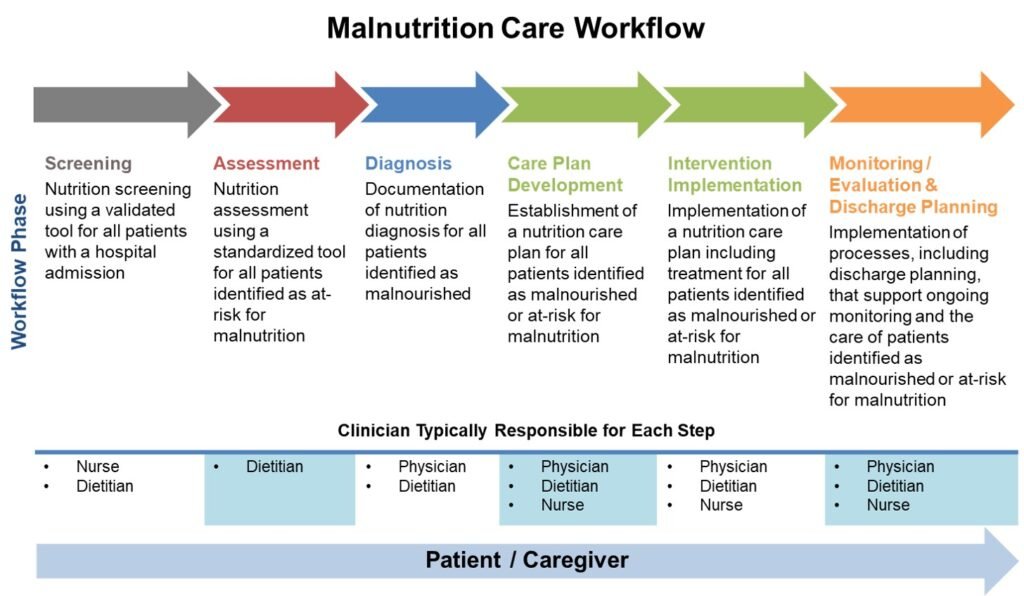
Identifying the signs and symptoms of malnutrition is essential for early detection and intervention. These indicators can vary depending on the severity and duration of malnutrition, as well as individual factors.
Physical signs of malnutrition
Physical signs of malnutrition can include noticeable weight loss, reduced muscle mass, thinning hair, dry skin, weak and brittle nails, and a swollen or bloated abdomen. Additionally, individuals may appear pale or have a dull complexion, as malnutrition can result in nutrient deficiencies that affect overall skin health.
Behavioral and psychological symptoms
Behavioral and psychological symptoms of malnutrition may manifest as changes in appetite, decreased interest in food, irritability, fatigue, difficulty concentrating, and a weakened immune system. Mood swings, depression, and anxiety can also occur as a result of nutrient imbalances affecting brain function.
Differentiating normal health issues and malnutrition symptoms
It is important to note that some signs and symptoms of malnutrition can overlap with other health issues. For example, fatigue and weight loss can be attributed to a variety of factors, including stress, lack of sleep, or underlying medical conditions. Therefore, it is crucial to consult a healthcare professional for a comprehensive assessment to determine the cause of these symptoms and identify if malnutrition is a contributing factor.
Clinical Assessment for Malnutrition
Clinical assessment plays a vital role in diagnosing and evaluating malnutrition. Healthcare professionals utilize several methods to gather relevant information and assess an individual’s nutritional status.
Initial medical history review
During an initial medical history review, healthcare professionals will inquire about an individual’s dietary habits, appetite, weight changes, digestive symptoms, and any underlying medical conditions that may impact nutrient absorption, metabolism, or utilization. Additionally, they will explore factors such as socioeconomic status, living conditions, and access to food.
Physical examination
A physical examination involves assessing an individual’s body composition, overall appearance, and any physical signs indicative of malnutrition. Healthcare professionals may examine the skin, hair, nails, and mucous membranes for signs of deficiency or other nutritional imbalances. Additionally, they may evaluate muscle mass, strength, and detect any swelling or fluid retention.
Assessment of dietary intake
Evaluating an individual’s dietary intake is crucial in determining nutrient deficiencies or imbalances. Healthcare professionals may use various methods, such as food diaries, to assess the types and amounts of foods consumed. These assessments provide valuable insights into the individual’s overall dietary patterns and help identify any deficiencies or excesses.
Laboratory Tests for Malnutrition
Laboratory tests complement clinical assessments and provide objective data to support a diagnosis of malnutrition. These tests help identify specific nutrient deficiencies, assess organ function, and detect any underlying medical conditions that may contribute to malnutrition.
Complete blood count (CBC) test
A complete blood count (CBC) test measures various components of the blood, including red and white blood cells, hemoglobin, and platelets. Anemia, which can be caused by iron, vitamin B12, or folate deficiencies, can be detected through the CBC test. Additionally, abnormal white blood cell counts may indicate an underlying infection or inflammation.
Serum proteins tests
Serum protein tests, such as albumin and prealbumin tests, assess the body’s protein status. Low levels of these proteins can indicate protein-energy malnutrition and a deficiency in essential amino acids. These tests provide insights into the body’s overall nutritional status and can help identify the severity of malnutrition.
Mineral and vitamin deficiency tests
Testing for specific mineral and vitamin deficiencies is essential in diagnosing malnutrition accurately. Blood tests can measure levels of various minerals, such as iron, calcium, and magnesium, as well as vitamins like vitamin D, vitamin B12, and folate. Nutrient deficiencies can have significant health implications, and identifying them allows healthcare professionals to prescribe appropriate treatment and interventions.

This image is property of pub.mdpi-res.com.
Anthropometric Measurements in Testing Malnutrition
Anthropometric measurements involve assessing an individual’s physical dimensions and body composition to determine nutritional status. These measurements provide valuable information about body fat distribution, muscle mass, and overall growth or wasting.
Body Mass Index (BMI) calculations
Calculating the Body Mass Index (BMI) is a widely used method to assess nutritional status and categorize individuals into underweight, normal weight, overweight, or obese. It is calculated by dividing an individual’s weight in kilograms by their height in meters squared.
Mid-upper arm circumference (MUAC) measurements
Mid-upper arm circumference (MUAC) measurements assess muscle mass and fat stores in the upper body. MUAC is a widely accepted indicator of nutritional status, especially in children. It is measured using a tape placed around the mid-upper arm, and the measurement obtained is compared to standard reference values.
Skinfold thickness measurements
Skinfold thickness measurements are used to estimate body fat percentage. This measurement involves using calipers to measure the thickness of skinfolds at specific sites, such as the triceps, biceps, or subscapular regions. The measurements are then used to estimate total body fat and assess nutritional status.
Dietary Assessment Techniques
Accurate assessment of an individual’s dietary intake is essential in diagnosing and addressing malnutrition. Healthcare professionals utilize various techniques to gather detailed information about an individual’s food choices, portion sizes, and overall nutrient intake.
24-hour dietary recall
The 24-hour dietary recall is a method in which an individual recalls all the food and beverages consumed within the past 24 hours. During the recall, healthcare professionals ask individuals to describe the type of food, portion sizes, and any condiments or extras consumed. This technique provides a snapshot of the individual’s typical dietary habits and allows healthcare professionals to identify any nutritional deficiencies or excesses.
Food frequency questionnaire (FFQ)
A food frequency questionnaire (FFQ) is a more extensive assessment tool that asks individuals to report how often they consume specific foods or food groups over a given period, such as a month or a year. This technique provides insights into long-term dietary patterns and allows healthcare professionals to identify any nutrient imbalances or deficiencies.
Diet history interview
A diet history interview involves a comprehensive conversation between the healthcare professional and the individual about their dietary habits, including likes, dislikes, cultural preferences, and any dietary restrictions or intolerances. This technique provides a holistic understanding of an individual’s relationship with food and helps identify any nutritional gaps or imbalances.
This image is property of www.verywellhealth.com.
Malnutrition Universal Screening Tool
The Malnutrition Universal Screening Tool (MUST) provides a systematic approach to screen individuals at risk of malnutrition. It is widely used in healthcare settings to identify individuals in need of further assessment and intervention.
Understanding MUST
MUST consists of three components: screening for BMI, unintentional weight loss, and acute disease effect. It categorizes individuals into low, medium, or high risk based on their scores in each component.
How to use the MUST tool
To use the MUST tool, healthcare professionals measure an individual’s height and weight to calculate the BMI. They inquire about any unintentional weight loss within the past three to six months and assess whether the individual has any acute disease or illness affecting their nutritional intake. Based on the scores obtained in each component, the individual is categorized into a risk group that informs the need for further assessment or intervention.
Interpreting and using MUST results
Interpreting MUST results allows healthcare professionals to identify individuals at risk of malnutrition and provide appropriate interventions. Those categorized as high risk require a comprehensive nutritional assessment and targeted interventions to meet their nutritional needs. Medium-risk individuals may benefit from dietary counseling and monitoring, while low-risk individuals can be monitored for any changes in nutritional status.
Utilizing the Subjective Global Assessment
The Subjective Global Assessment (SGA) is a comprehensive method for evaluating an individual’s nutritional status based on medical history, physical examination, and clinical judgment. Healthcare professionals utilize SGA to assess an individual’s nutritional risk and guide interventions.
Understanding subjective global assessment
SGA considers both subjective and objective data to assess nutritional status. It involves a detailed medical history review, physical examination, and careful evaluation of the individual’s overall clinical condition.
How to conduct a subjective global assessment
Conducting a subjective global assessment involves obtaining a detailed medical history, including information about weight changes, appetite, presence of gastrointestinal symptoms, and current medical conditions. A physical examination is then conducted, focusing on body composition, muscle wasting, and signs of nutrient deficiencies.
Analyzing subjective global assessment results
Analyzing the results of SGA allows healthcare professionals to identify the individual’s nutritional risk. Those classified as well-nourished require standard nutritional care, while individuals at moderate risk may require dietary counseling and monitoring. Those categorized as severely malnourished require intensive nutrition interventions, such as enteral or parenteral feeding, to address their nutritional needs.
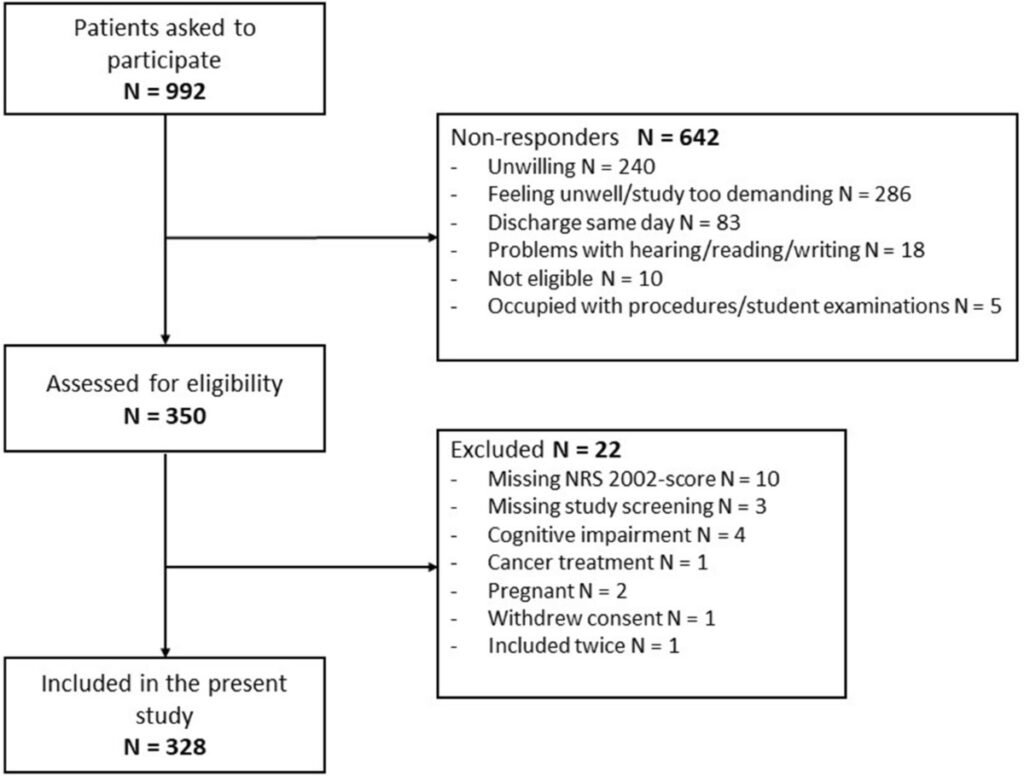
This image is property of media.springernature.com.
Nutrition-Focused Physical Exam
A Nutrition-Focused Physical Exam (NFPE) provides a detailed analysis of an individual’s physical appearance, body composition, and organ systems to assess their nutritional status. This comprehensive evaluation helps healthcare professionals identify nutrient deficiencies, signs of malnutrition, and guide appropriate interventions.
Concept of nutrition-focused physical exam
NFPE focuses on physical examination findings that are directly related to nutritional status. It involves assessing the skin, nails, eyes, oral cavity, muscles, and fat stores to identify potential nutrient deficiencies, malnourishment, or other signs of poor nutrition.
How to conduct a nutrition-focused physical exam
During a nutrition-focused physical exam, healthcare professionals assess an individual’s overall appearance, signs of dehydration, skin health, muscle wasting, edema, evidence of nutrient deficiencies (such as pale conjunctiva indicating iron deficiency), and other physical signs indicative of malnutrition.
How to interpret the findings of a nutrition-focused physical exam
Interpreting the findings of an NFPE allows healthcare professionals to identify specific nutrient deficiencies or malnutrition and provide targeted interventions. The results can guide dietary modifications, the inclusion of nutritional supplements, or referrals to other healthcare professionals for further assessment and management.
Malnutrition Prevention and Treatment
Preventing and treating malnutrition requires a multi-faceted approach that includes nutrition education, dietary adjustments, supplementation, and medical interventions as necessary.
Nutrition education and counseling
Nutrition education plays a crucial role in preventing malnutrition by providing individuals with the knowledge and skills needed to make healthy food choices and meet their nutritional needs. Healthcare professionals can provide personalized dietary recommendations and offer guidance on meal planning, portion control, and addressing any dietary restrictions or preferences.
Dietary adjustments and supplementation
Dietary adjustments are often necessary to address specific nutrient deficiencies or imbalances. This may involve increasing the intake of nutrient-dense foods such as fruits, vegetables, whole grains, lean proteins, and healthy fats. In cases where dietary modifications alone are insufficient, nutritional supplements may be prescribed to provide additional nutrients.
Medical treatment and interventions
In severe cases of malnutrition, medical treatment and interventions may be required to address underlying conditions, restore nutrient balance, and support overall health and recovery. This may involve hospitalization, enteral or parenteral nutrition (feeding via a tube or intravenously), and close monitoring by healthcare professionals to ensure adequate nutrition and progress.
In conclusion, understanding malnutrition is crucial for proper diagnosis, intervention, and prevention. Recognizing the signs and symptoms, conducting clinical assessments, using laboratory tests and anthropometric measurements, and employing dietary assessment techniques can help identify malnutrition and guide appropriate interventions. Tools like MUST, SGA, and NFPE aid in the screening, assessment, and evaluation of nutritional status, providing a comprehensive approach to address malnutrition. Prevention and treatment of malnutrition require a combination of nutrition education, dietary adjustments, supplementation, and medical interventions to restore nutritional balance and promote overall health and well-being.